In America a head injury is the cause of most deaths aged 15-44 years and is the third leading cause of death overall. In developing countries such as Indonesia, along with advances in technology and development tend to be increasing in frequency. Head injury contributes to nearly half of all deaths due to trauma, given that the head is the most common and vulnerable sections involved in an accident. (1,3,4)
Distribution of cases of head injury, especially involving the productive age group of between 15-44 years, with a mean age - average about thirty years, and is dominated by the men - men rather than women. The most common causes are traffic accidents (49%) and then followed by falls (especially in the age group of children - children). (1,3,4)
In daily life - the head injury is a common challenge for the medical community to deal with it, where it seems the sustainability of pathophysiological processes disclosed with all the latest medical breakthroughs Diagnostics investigations tend not something simple. Various long term as kromosio and contusions now ditingalkan and calcification head injury is more leads in the application of clinical management in achieving maximum success of treatment. (1)
Injury to the head may involve all layers of the structure, from the layers of the scalp or the lightest level, skull, durameter, vascular brain, until the brain tissue itself. Whether in the form of a closed wound, and penetrating trauma. With the understanding of the pathophysiology foundation-detailed biomekanisme of each - each process above, who are faced with handling procedures quickly and accurately, is expected to reduce morbidity and mortality. (1)
Types of mechanical loads on the head so varied and complicated. In outline grouped into two types: static load and dynamic loads. Arising static load slowly - in this case the land force applied to the head pressure gradually, it can happen when the head of the gencetan or slow the effects of pressure and takes place in a time period of more than 200 milliseconds. May lead to bone fractures, multiple fractures, or base of the skull or bones kominutiva tengkorak.Biasanya coma or neurologic deficits typical yet appeared, except when extreme deformation of the skull, causing compression and distortion of brain tissue, and subsequently suffered fatal damage. (1 )
Ruda mechanism forced the more common is due to dynamic loads, in which these events take place in a shorter period of time (less than 200 milliseconds). This load is divided into shock loads and load impact. This incident can be a complication of intracranial hematoma, which can make patients with mild head injury in a short period of time included in an objec severe and life-threatening.
On one hand it is only partially head injury cases that come to the hospital continues to be a hematoma, but on the other hand "the frequency of hematoma is present in 75% of cases that come out consciously and died". (1,3)
II. ANATOMY
1I.1 meninges and Vasa Blood Brain
1. meninges
The meninges are connective tissue sheath that wraps the non Sarafi brain and spinal cord that barisi cerebrospinal liquor and serves as a schock absorber. The meninges consist of three layers from outside into that: the dura mater, and piamater Arachnoidea. (1,3,4)
a. dura mater
Is a dense membrane, hard and inelastic. Dura mater of the spinal cord wrapping consisting of a sheet, while the dura mater of the brain consists of two sheets are laminated endostealis which is a fibrous connective tissue cranium, and lamina meningealis. Folds / duplikatur in some places, which is the median between the two hehemispherium dilinea called falx cerebri cerebri, which is a triangular continuation of the falx cerebri kekaudal called Falx cerebelli, which is a tent-shaped roof of the posterior fossa skull separates the cerebrum with the cerebellum called the tentorium cerebelli, and sheet covering the sella tursica is wrapping hipophysis called diaphragm sellae. (1,3)
Between two pieces of the dura mater, in some places forming the room called sinus (venous) duramatris.
Sinus duramatis receives flow from vv. Cerebri, vv. Diploicae, and vv. Emissari. There are two kinds of sinus duramatis single and paired. Single dural sinuses are: superior sagittal sinus, inferior sagittal sinus, sinus rectus, and occipital sinuses. Superior sagittal sinus receives blood from the veins. Cerebri, vv. Diploicae, and vv. Emissari.Sinus inferior sagittal receives blood from the brain medial facies. Sinus rectus located between the falx cerebri and tentorium cerebelli, a continuation of v. magna cerebri, the superior sagittal sinus confluens sinuum form. Occipital sinus from the foramen magnum, join confluens sinuum. (1)
Sinus dural sinuses are paired tranversus, cavernous sinus, sinus sigmoideus and the superior and inferior petrosal sinuses. Tranversus sinus receives blood from the superior sagittal sinus and sinus rectus, and then flows into v. internal jugular. Sinus sinus tranversus sigmoideus is an advanced form of the letter S. The superior and inferior petrosal sinus receives blood from the cavernous sinus and draining each - each to sinus traaanversus and v. internal jugular (1)
b. Aracnoidea
Delicate membrane adjacent to the dura mater, does not enter into the sulcus / fissure except longitudinal fissure. Of the many emerging trabecula aracnoidea gently towards building such kepiamater forming webs - profit.
Among aracnoidea and there piamater subaracnoidale spatium space, which in some places formed cisterna widened. While the narrow gap between the dura mater and aracnoidea called spatium subdurale, narrow slits called spatium epidurale outside the dura mater.
From aracnoidea also appears flakes - flakes were held invagination called the dura mater to granulasio aracnoidales especially sagittal sinus area which serves a one-way valve allows her materials - materials from the CSF into the venous sinuses. (1,3)
c. Piamater
Piamater firmly attached to the brain and spinal cord, following every curve, containing small vasa. Certain place along with the ependyma form choroidea tela. Piamater acts as a barrier against the entry of harmful compounds. (1,3)
II.2. Vasa Blood Brain
a. arteries
Brain divaskularisasi by branch - a branch. and the internal carotid a. vertebral. A. is a branch of the internal carotid a. carotid comunis the skull into the cavity through the carotid canal, branches are a. optalmica, a. choroidea anterior, a. cerebralis anterior and medial a.cerebralis. A. opthalmica mempercabang a. centralis of the retina, a. cerebralis anterior ramify a. communicans anterior, whereas a. cerebralis medialis ramify a. communican posterior. (3)
Vertebral artery is a branch. subclavian up to the neck through the foramina tranversalis. Both a. The cranial vertebral forming a puncher. basillaris which ramify aa. Pontis, a.labirintina (following n. V and n. VIII), a. cerebellaris superior (as high as n. III and n. IV) and a. cerebralis posterior which is a terminal branch. basilar. (3)
-.cabang A branch. and the internal carotid a. vertebral shape circulus arteriosus of Willis which are around the chiasma opticum. Formed by a. cerebralis anterior, a. cerebralis media, a. cerebralis posterior, a. comunican posterior and anterior a.communican. This system allows the blood supply to the brain is inadequate, especially in case of occlusion / blockage. (3)
b. Veins
Veins tampered dikalsifikasikan as follows: (3)
- Vena cerebri externa, covering v. cerebralis superior / lateral / medial / inferior and vv. Basallles.
- The internal cerebral veins, covering v. choroidea and v. cerebri magna.
- Vv. Cerebellaris
- Vv. Emissariae, the dural venous sinuses that connect the superficial veins to the cranium which serves as a pressure valve in case kenaiakan intracranial pressure. Also plays a role in the spread of infection into the skull cavity.
Veins from the truncus cerebri and cerebellum generally follow the flow of the artery. While the backflow of blood in the cerebrum venosa not not follow the pattern in the arteries. All of the blood leaving the brain through the venosa v. internal jugular on the skull base. Anastomosis is very extensive and effective venosa between vv. Superficial and vv. Deep in the brain. (3)
III. CLINICAL aplikas
In head injury can occur in intracranial hemorrhage / hematoma intracranial divided into: a hematoma which is located outside the dura mater is
epidural hematoma, and which is located within the dura mater is the subdural hematoma and intracerebral hematoma; each of which can occur alone or besamaan. (3)
III.1 Epidural Hematoma
III.1.a. definition
Epidural hematoma is a collection of blood between the skull to the dura mater (known as extradural hematoma). This type of hematoma is usually derived from arteriel bleeding due to a linear fracture that causes a direct laceration or tear arteries meninges (a. Meningeal). Accompanying skull fracture was found in 8% - 95% of cases, while the rest (9%) due to the strain and tear the artery without any fracture (especially in the case of children where the deformity that occurs only temporarily). Epidural hematoma derived from venous bleeding occurred less frequently. (1,3,5)

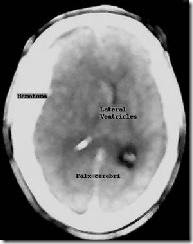
Figure CT SCAN epidural hematoma
Etiology III.1.b
Movement which led to the epidural hematoma include: (5)
head trauma
Cutouts a / v meningeal median
Rupture sagittal sinus / sinus tranversum
Rupture v diplorica
This type of hematoma is usually derived from an arterial bleeding due to linear fractures that cause direct laceration or tear of the middle meningeal artery mediana.Fraktur accompanying skull found 85-95% of cases, while the rest (9%) due to the strain and tear the artery without any fracture, especially in cases of children where the deformity that occurs only temporary. (1,3)
This type of hematoma derived from venous bleeding is less common, usually caused by a sinus laceration by fracture duramatris occipital, parietal or sphenoid bone. (1,3)
III.1.c. classification
Based on the chronology of epidural hematoma is classified into (1.3)
1. Acute: diagnosis determined within 24 hours after trauma
2. Subacute: diagnosis determined between 24 hours - 7 days
3. Chronic: diagnosis specified day 7
III.1.d. pathophysiology
Epidural hematoma occurs due to blunt force head injury and in a slow time, such as a fall or hit something, and it is almost always associated with linear cranial fracture. In most patients, bleeding occurs in the middle meningeal artery, vein, or both. Middle meningeal blood vessel injury ketikaterjadi indentation fracture line passes minengeal the temporal squama.
III.1.e. clinical symptoms
Clinical symptoms of epidural hematoma consist of tria symptoms;
1. Interval lusid (free interval)
After a short period of unconsciousness, no lucid interval followed by adverse developments in consciousness and contralateral hemispheres. More than 50% of patients did not reveal any lucid interval, and unconsciousness that occurs from the time of the injury.
Headache is a very common illness, due to the opening of the dura from the inside of the cranium, and usually progressive if there is a lucid interval.
Lucid interval may occur in minimal parenchymal damage. This interval describes the time between the unconscious and the first suffered from trauma and chaos at the start of the diencephalic due to transtentorial herniation. The length of the short lucid interval which allows for possible bleeding comes from the arteries.
2. Hemiparesis
Neurological disorders are usually collateral hemipareis, depending on the magnification effect of mass on corticispinal area. Ipsilateral hemiparesis until penjendalan can also cause pressure on the contralateral cerebral peduncle at territorial level.
3. Anisokor pupils
Ie ipsilateral dilated pupil. In perjalananya, pupil dilation and will reach a maximum at the beginning of the light reaction is positive to negative. There is also a rise in blood pressure and bradikardi.pada last stage, decreased consciousness to deep coma, pupillary dilation contralateral also experienced until both pupils showed no reaction to light again which is a sign of death.
III.1.f. therapy
Epidural hematoma is surgically for evacuation as soon as possible, decompression of the brain tissue underneath and address the source of bleeding.
Usually mounted postoperative drainage for 2 x 24 hours to avoid new yamg blood collection.
- Trepanation -kraniotomi, hematoma evacuation
- Craniotomy-evacuation of hematoma
III.1.g. Complications and Outcome
Complications of epidural hematoma can provide:
Cerebral edema, is a state-pathological symptoms, radiologic, and appearance-operative Ntra which this state has a very significant role in the occurrence of brain shift (brain shift) and increase intracranial pressure
Brainstem compression - died
While the outcome on epidural hematoma, namely:
Mortality was 20% -30%
Heal with neurologic deficits of 5% - 10%
Recovered without neurologic deficit
Live in a vegetative state conditions
III.2 subdural hematoma
III.2. a definition
Subdural hemorrhage is bleeding that occurs between the dura mater and the arachnoid. Subdural hemorrhage can be derived from:
1. Ruptured venous bridge ("Bridging vein") which is a vein that runs from the subarachnoid space or subdural space across the cerebral cortex and empty into the venous sinuses of the dura mater.
2. Tear cortical blood vessels, subarachnoid, or arachnoid
Subdural hematoma CT SCAN Image
III. 2. b Etiology
1. Head trauma.
2. Arteriovenous malformation.
1. blood dyscrasias.
2. Anticoagulant Therapy
III.2.c. classification
1. Acute Bleeding
The symptoms soon for hours - hours after trauma.Biasanya occur on a fairly severe head injury that can lead to deterioration over
continued in patients who are usually already disturbed consciousness and vital signs. Bleeding can be less than 5 mm thick but widely dilated. In the picture skening tomografinya, obtained hiperdens lesions.
2. Bleeding subacute
Develop within a few days usually about 2-14 days after the trauma. In this sub-acute subdural found a mixture of blood clots and fluid blood. Bleeding can be thicker but no formation of the capsule around it. In the description of the lesions obtained skening tomografinya isodens or hipodens.Lesi isodens obtained because the lysis of red blood cells and resorption of hemoglobin.
3. Chronic Bleeding
It usually occurs after 14 days after trauma could even chronic subdural lebih.Perdarahan, symptoms can appear within weeks or months after a mild trauma or traumas that are not clear, even a mild hit can result in subdural hemorrhage if the patient also experienced vascular disorders or clotting disorders. In chronic subdural hemorrhage, we must be careful because these hematomas over time can
become gradually enlarges, resulting in suppression and herniation. In chronic subdural, found the capsule of connective tissue formed around the hematoma, the newer, or the capsule is still not formed a thin surface area Arachnoidea. The capsule is attached to araknoidea if there is a tear in the lining of the brain. This capsule is containing blood vessels are thin walls, especially on the side of the dura mater. Because of this thin wall proteins from blood plasma can penetrate and increase the volume of the hematoma. These blood vessels can rupture and cause bleeding which led to new menggembungnya hematoma. Blood in the capsule will form a viscous liquid that can suck the liquid from room subaraknoidea. Hematoma will grow and cause symptoms of cerebral tumor bleak. In most chronic subdural hematoma was found in patients aged over 50 years. In the description of hypodense lesions obtained skening tomografinya
III. 2.d. pathophysiology
Cortical vein toward the dura or dural sinus pecahdan bruising or laceration, is a common site of bleeding. It is highly associated with comtusio cerebral and brain edema. CT scan showed a mass effect and midline shift in exsess of thickness yamg hematoma associated with brain trauma.
III. 2.e. clinical symptoms
Clinical symptoms vary from mild (headache) to penutunan consciousness. Most subdural hematoma consciousness is not so great deperti primary neuronal injury cases, except when there is a mass effect or other lesions.
The symptoms are not typical and meruoakan manifestation of elevated intracranial pressure such as headache, nausea, vomiting, vertigo, papilledema, diplopia due to paralysis n. III, epilepsy, anisokor pupil, and neurological deficits lainnya.kadang trauma when the history is not clear, often suspected brain tumor.
III.2.f. therapy
Action therapy in these cases is the immediate craniotomy with evacuation of the hematoma via burr-hole irrigation. Specifically in patients with chronic subdural hematoma of old age which usually have a thick capsule hematoma and brain tissues are already experiencing atrophy, usually more advisable to perform a craniotomy surgery (diandingkan with burr-hole course).
III.2.g. Complications and Outcome
Subdural hematoma can provide complications include:
1. Hemiparesis / hemiplegia.
2. dysphasia / aphasia
3. Epilepsy.
4. Hidrosepalus.
5. Subdural empyema
Outcomes for subdural hematoma Sedangaka are:
1. Mortality in Acute subdural hematoma around 75% -85%
2. In sub-dural hematoma chronic:
- Cured without
 neurological impairment about 50% -80%.
neurological impairment about 50% -80%. - Cured with neurological disorders approximately 20% -50%.
III.3 intracerebral hematoma
III.3.a. definition
Is bleeding that occurs within the brain tissue. Post-traumatic hematoma intraserbral merupkan focal collection of blood usually strain or tear caused injury to the vessels rational brain darahintraparenkimal or sometimes injury penetrans. The hematoma size varies from a few millimeters to several centimeters and can occur in 2% -16% of cases
of injury.
Intracerebral hematoma refers hemorragi / bleeding over 5 mldalam substance of the brain (hemorrhage
smaller called punctate or petechial / patches).
Figure CT SCAN intracerebral hematoma
III.3.b. etiology
Intracerebral hematoma can be caused by:
1. Head trauma.
2. Hypertension.
3. Arteriovenous Malformation.
4. aneurysm
5. Anticoagulant Therapy
6. Blood dyscrasias
III.3.c. classification
Classification of intracerebral hematoma by location;
1. Hematoma tentoral supra.
2. Hematoma serbeller.
3. pons-brainstem hematoma.
III.3.d. pathophysiology
Intracerebral hematoma biasanta 80% -90% are located in the frontotemporal region or in the basal ganglia, and is often accompanied by other primary neuronal lesions and fractures calvaria.
III.3.e. The clinical symptoms.
Clinical patient is not so typical and frequent (30% -50%) remained conscious, extra axial hematoma is similar to the other. Clinical manifestations in peak appears after 2-4 days post-injury, but with the computer tomography scan of the brain
diagnosis can be established more quickly.
Criteria for diagnosis of hematoma supra tentorial
sudden headache
decreased level of consciousness within 24-48 hours.
Focal signs that may occur;
- Hemiparesis / hemiplegi.
- Hemisensory.
- Hemi anopsia homonym
- Parese nerve III.
Criteria for diagnosis of hematoma serebeller;
Acute headache.
Impairment of consciousness.
ataxia
Signs of elevated intracranial pressure.
Criteria for diagnosis of pontine brainstem hematoma:
Impairment of consciousness coma.
Tetraparesa
respiration irregular
Pupil pint point
pyrexia
Diskonjugat eye movements.
III.3.f. therapy
For small hemmoragi treatmentnya is observational and supportive. Blood pressure should be monitored. Hypertension can accelerate the onset of hemmoragi. Intra-cerebral hematoma can be treated with a broad hyperventilation, mannitol and steroids with monitorong intracranial pressure as uasaha to avoid surgery. Surgery is performed for a broad and massive hematoma patients with neurological chaos or elevation of intracranial pressure due to medical therapy
conservative
If the bleeding is more than 30 cc supratentorial
If the bleeding is less than 15 cc celebeller
When the brain stem pontine haemorrhage.
surgery
craniotomy
- If bleeding supratentorial over 30 cc with mass effect
- If bleeding cerebeller over 15 cc with mass effect
III.3.g. Complications and Outcome
Intracerebral hematoma can provide such complications;
Cerebral edema, brain swelling
Brainstem compression, dies
While the outcome of intracerebral hematoma can be:
Mortality was 20% -30%
Recovered without neurological deficit
Cured premises neurological deficits
Live in a vegetative state conditions.
IV. CLINICAL EXAMINATION OF HEAD INJURY
Clinical examination is the most comprehensive examination of the diagnostic evaluation of patients suffering head injury, where the examination of serial = rapid and noninvasive tepa expected to nenunjukkan progression or deterioration of the disease or the disorder. Relative incidence of abnormalities tinnginya / concomitant systemic injuries (over 50%) in cases of severe head injury, it is necessary to note the following;
level of consciousness
The level of consciousness was assessed by Glasgow scale (GCS "Glasgow Coma Scale). This is a simple grading scale of "arousal" and the functional capacity of the cerebral cortex based on verbal response, motor and eye sufferers.
Best motor response
|
|||||||
6
|
Following orders
|
||||||
5
|
Pain localized to the
|
||||||
4
|
Occurs withdrawal effects of pain
|
||||||
3
|
abnormal flexion
|
||||||
2
|
extension abnormal
|
||||||
1
|
There is no movement
|
||||||
The best verbal
response
|
|||||||
5
|
Oriented and
precise
|
||||||
4
|
The conversation
confusing
|
||||||
3
|
improper
|
||||||
2
|
The sound is not
understandable
|
||||||
1
|
do not
|
||||||
Opening eyes
|
|||||||
4
|
spontaneous
|
||||||
3
|
against the
conversation
|
||||||
2
|
To pain
|
||||||
1
|
There is no eye
opening
|
||||||
2. The movement of the eyeball
Eyeball movement is an important index for the assessment of functional aktiffitas brainstem (rektikularis formation). Patients who are fully aware (alert) and has a good eye ball movement signifies intaknya motorikokuler system in the brain stem. On the declining state of consciousness, voluntary eye movements disappear, so as to assess the movement of the reflex okulosefalik determined and okulovestibuler.
pupil
Assessment pupil size and response to light stimuli is important in dealing with the initial examination of a head injury.
One of the early symptoms of herniation of the temporal lobe are dilated and pupillary light response slowing. In this case the compression and distortion when the oculomotor nerve tentorial herniation unkal events will disrupt axon funsi parasympathetic efferent signals to deliver konstrksi pupil.
Pupillary changes in epidural hematoma can be seen from the table

motor function
Usually only a complement to remember sometimes difficult to get an accurate assessment of patients with loss of consciousness. Each limb was graded strength with the following scale:
Normal: 5
Moderate decline: 4
Decreased weight (can defy gravity): 3
Unable to resist gravirasi: 2
Slightly move: 1
No movement: 0

On behalf of myself and my family, I would like to thank the doctor who saved my father’s life, Dr. Aparajita who was kind enough to send Remedium product during a difficult time, It was overwhelmed to read how many people cared and that they were thinking of my dad and willing his recovery. This was a scary time for us because he was very forgetful and needed to be transported to therapy 30 minutes away twice a week. He was also taking Dilantin, for seizures, though thankfully he no longer needs to take it. We met the neurosurgeon at 17:00 hours and he went on to explain what had happened. He mentioned that he had an aneurysm that ruptured and would need to have surgery to clip the blood vessels. The term he used was subarachnoid hemorrhage. The operation was scheduled for the 9th May 2017 at 09:00 hours. It was to last for 3 hours. I was lucky to come across a lady who was cured from brain hemorrhage through Herbal Medication while at work. I contacted Aparajita through an email address I got from her. Without further delay I made an order, I switched my father over to it. He had a great breakthrough, that in the second month, we were already testifying of the effective of the Herbal medication. After eight months course of taken the medicine, all symptoms were gone.
ReplyDeleteHe started doing full time work around the end of the summer and some days were better than others. My manager and the entire company have been very understanding about his recovery as I was always there for him. There were days he get head pains and I worry about that, but Dr. Aparajita said it would continue healing for 8months of taken his herbal medicine. My father used to get tired so easily but this Product really helped his anxiety, as well as, tiredness. This whole ordeal left me shaken and extremely thankful for him to be alive, in the condition I am in. I thank God, I thank Dr. Aparajita, my wonderful husband Newman, my family, workplace, friends and co-workers who guided me back to order Remedium product which put my father to where he is today one year later. He now gets his energy and strength back and to the person he was before as I can. He miss being able to hike and hope he get back to doing that. He's a lot more understanding of those around him and try to relax more and not take things too seriously anymore. If you can die at any moment what is important to you? For me, it’s those I love (Family). Everything else will work itself out.
It has been 1 year and four months since I became free from brain hemorrhage. Anyone who is not in my position would not understand what he went through, the heart break, the pain and how frustrated he was for 6 odd years. Believe me, it was hell. I am so happy; I never believed I will be this happy again in life. His story is quite lengthy, it might help you too. You may contact Dr. Aparajita to know more via his email on. aparajitatan@gmail.com
Very well written article mate, thank you for the valuable and useful information. Keep up the good work! FYI, please check these depression, stress and anxiety related articles:
ReplyDeleteDepression Cure
10 Things That Really Won’t Cure My Depression
Depression Quotes
Myths and Facts about Depression
Depression Facts
You can also contact me at depressioncure.net@gmail.com for link exchange, article exchange or for advertisement.
Thanks
Vik.